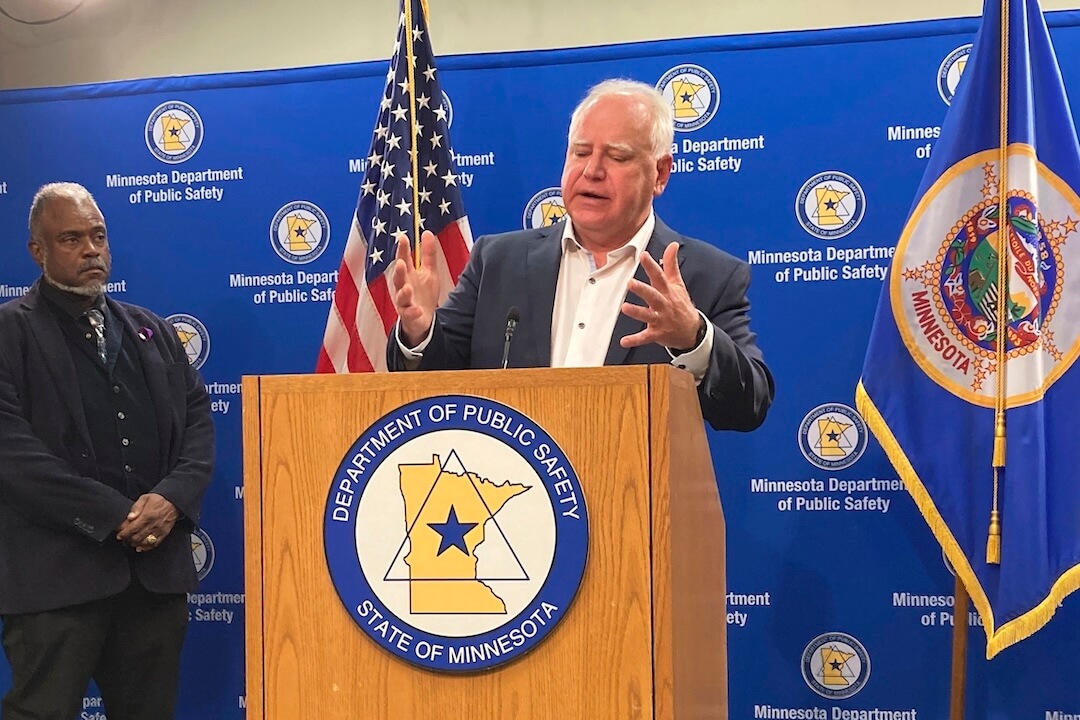
Shortly after Vice President Kamala Harris tapped Minnesota Gov. Tim Walz to be her presidential running mate, he faced increased scrutiny over how he led his state during the coronavirus pandemic’s apex.
One claim is that a Minnesota health department program that sought to ensure equitable distribution of monoclonal antibody treatments discriminated against white people.
“During Covid, Tim Walz rationed access to monoclonal antibody treatments based on skin color. Being non-white gave a person more priority than having hypertension, and was equal in importance to having massive risk factors like diabetes or cardiovascular disease,” conservative political activist Charlie Kirk wrote Aug. 6 on Threads. “How many people did Walz kill because he thought they were less deserving due to their race?”
We contacted a Kirk spokesperson for evidence supporting his claim but received no response.
We also found other social media posts making the same claim.
The notion that access to the treatments was rationed by race and that may have led to the deaths of white people is false and ignores key details about Minnesota’s policy, experts told PolitiFact.
The Minnesota Department of Health said the Food and Drug Administration acknowledged that race and ethnicity “may also place individual patients at high risk for progression to severe COVID-19.” That risk may not be determined by underlying conditions alone, possibly because of underdiagnosis of other diseases in Black, Indigenous and people of color populations.
To account for that, Minnesota developed a scoring system that factored in race to determine who would be prioritized for the antibody treatments. This system was in effect for about one month of the program’s 16-month duration.
The state had abandoned the scoring system by the time a weighted lottery system was needed when monoclonal antibody treatment supplies were lowest.
A November 2023 case study showed that at least 79% of the people the program referred to get monoclonal antibody treatments were white. White people constitute 77% of the state’s 5.7 million-person population.
The Harris-Walz campaign defended Walz’s pandemic actions as governor.
“Americans haven’t forgotten that at the height of the pandemic, states were forced to ration treatments for COVID-19 because Donald Trump failed to deliver the resources to keep our families safe and healthy,” Sarafina Chitika, a campaign spokesperson, said in an email. “As Governor, Tim Walz made sure treatments for COVID were delivered to patients who needed them most in order to save as many lives as possible despite Trump’s failures.”
What happened in Minnesota?
Monoclonal antibody treatments use laboratory-made proteins that mimic a person’s immune system to fight off viruses. The U.S. Food and Drug Administration granted emergency use authorization as early as November 2020 for several of these products to treat COVID-19. These treatments, administered in outpatient settings, helped reduce the risk of COVID-19-related hospitalization and death.
Monoclonal antibody treatments were sometimes in short supply during pandemic surges. Minnesota in February 2021 launched the Minnesota Resource Allocation Platform, a program to equitably connect patients with the treatments based on clinical need. The program ran from Feb. 9, 2021, to July 1, 2022.
The goal, said J.P. Leider, a University of Minnesota associate public health professor who helped lead the project, was to have a centralized system to give any Minnesotan access to the treatments based on clinical data, rather than a first-come, first served policy that many states used.
The policy involved prioritizing access to the treatments. It first prioritized referrals for the treatment based on FDA criteria for identifying high-risk patients laid out in the agency’s emergency use authorizations, which changed over time. Besides multiple health conditions, the FDA said in May and July 2021 that race or ethnicity may place patients at “high risk for progression to severe COVID-19” partly because of other potentially undiagnosed health concerns.
Minnesota later designed a scoring system first used in December 2021 that assigned people points, on a scale of zero to 25, based on categories of clinical risk from COVID-19, The program used the Mayo Clinic’s Monoclonal Antibody Screening Score, but added categories for pregnant women and Black, Indigenous and people of color as risk factors.
The state’s Health Department said the score was adapted after studies showed pregnant women and Black people, Indigenous people and people of color “were independently associated with poor clinical outcomes from COVID-19 infection.”
Minnesota’s scoring system awarded:
- Four points: to pregnant women; patients who are immunocompromised.
- Three points: to people with chronic kidney disease; patients 55 years and older with chronic respiratory disease.
- Two points: to people ages 65 years or older; people with body mass indexes of 35 kg/m2 and higher; people with diabetes; cardiovascular disease in a patient 55 years and older; Black, Indigenous or people of color status.
- One point: to patients 55 years and older with hypertension, which is also known as high blood pressure.
Race alone wouldn’t put people in the highest priority group unless they were older or had other risk factors.
Some critics and legal scholars questioned Minnesota’s approach at the time.
Eugene Volokh, a UCLA law professor who criticized Minnesota’s policy in a 2022 essay, told PolitiFact that considering race in rationing medical care “would generally be unconstitutional.”
“I set aside unusual situations where race is directly medically relevant — for instance, if some medicine works well for East Asians but not for whites, or some such. That, as I understand it, was not at all relevant to COVID treatments.”
Minnesota on Jan. 12, 2022, removed race as a scoring factor for the rest of the program amid complaints about discrimination and threats of a lawsuit by America First Legal, a group started by Stephen Miller, once an adviser to former President Donald Trump. Objections to using race as a factor in treatment allocation were also raised in Utah and New York.
Scores for other health risks remained unchanged in Minnesota’s program, although pregnancy was also removed as a factor because pregnant people “are clinically prioritized, independent” of their score, the health department said.
The state, in its announcement, did not explain why Black, Indigenous or people of color status was removed as a scoring factor. The Minnesota Department of Health did not return PolitiFact’s request for comment.
Dan Wikler, a Harvard University ethics and population health professor, said pandemic-era points systems for weighing allocation of life-saving resources, such as vaccines and therapeutics, arose after debate among health professionals and usually came from institutions such as universities or the Mayo Clinic in Rochester, Minnesota. Other institutions then adapted these systems, he said; this is what happened in Minnesota. The state’s scoring system was adapted from the Mayo Clinic’s system.
It’s “ludicrous” to attribute those health plans to Walz or any other governor, Wikler said.
“Very few would have had any idea of what was going on in these debates, and surely would have been unable to tell you what the guidelines for these institutions were,” he said.
Wikler said the debates centered on balancing twin goals — using resources to do the most good and ensuring that everyone had a fair chance to benefit.
“There is no way to honor both of these goals fully. Among those contributing to the discussion of the ethics of these choices, people of good will often reached very different conclusions,” Wikler said.
Why was race initially used?
Minnesota’s health department cited the FDA’s guidance in 2021 emergency-use approvals for monoclonal antibody treatments that “in addition to certain underlying health conditions, race and ethnicity “may also place individual patients at high risk for progression to severe COVID-19.”
That “acknowledgment means that race and ethnicity alone, apart from other underlying health conditions, may be considered in determining eligibility for (monoclonal antibodies),” the health department said in its “ethical framework” about allocation of the treatments.
“That was based on scientific evidence at the population health level that was showing us every single day that Black people and Latino people were experiencing worse symptoms and were more likely to be hospitalized and more likely to die from the COVID-19 virus,” University of Minnesota health and racial equity professor Rachel Hardeman said.
Provisional age-adjusted Centers for Disease Control and Prevention data shows that Black people; Hispanics; American Indian or Alaska Natives; and Native Hawaiians or Pacific Islanders all had higher COVID-19 death rates than whites. American Indians and Alaska Natives were about twice as likely to die from COVID-19, and Hispanic, Black, Native Hawaiian and Pacific Islanders were about 1.5 times as likely to die.
Hardeman said those disparities were worse during the pandemic’s height.
“In Minnesota, for instance, in January of 2022 we saw that Black people, while just comprising about 6% of the population in Minnesota, were actually 11% of the COVID-19 hospitalizations for quite some time,” Hardeman said. “Certainly those numbers fluctuated, but there was always consistently a gap based on race, which is why this decision was made.”
Does that mean white people were discriminated against?
Kirk’s claim that Minnesota rationed health care by skin color has elements of truth in that a scoring system awarded patients who were Black, Indigenous or people of color 2 points, the same as patients with diabetes or cardiovascular disease and more than a patient with hypertension.
But it ignores several facts and implies, with no evidence, that the scoring system led to deaths of white people.
“I don’t have data that shows that (the program led to white people dying). I don’t have reason to think that,” Leider, the public health professor, said. “What I’ll say about the state of Minnesota is that we set up a system where anybody could come in and get a referral. Didn’t matter if they had a doctor who knew about this or not, and because of the demographics of our state that we are, especially in the older group, whiter, I think that our system demonstrably prevented hospitalizations and hopefully saved lives, compared to a lot of the other states that were just letting it be first come first serve.”
Leider pointed to a 2022 study of Medicare patients that showed nationwide, people with no chronic diseases were five times likelier to receive monoclonal antibody treatments than people with six or more chronic conditions.
A 2022 Centers for Disease Control and Prevention report also showed much lower use of the treatments among Black, Asian, Hispanic and other races compared with white patients.
Dr. Monica Peek, a University of Chicago professor for health justice of medicine, said some public health officials used race as a proxy for exposure to racism, which she said limits access to goods and services and increases exposure to risks and harms. Racialized minorities, she said, have increased risk for chronic diseases and were at an increased risk for COVID-19 exposure. Many front-line workers who had increased risk of contracting COVID-19, such as hospital and grocery store workers, were Black and brown, she said.
The attempts to “try to mitigate the exposure to racism when we’re trying to allocate resources is really an attempt to mitigate the harm that racial and ethnic minorities have been exposed to,” Peek said. “And so it’s not trying to increase the harm for white people. It’s trying to decrease the harm for Black and brown people.”
States and cities used different strategies to equitably allocate resources fairly and ensure populations most at risk received resources first, using factors such as chronic diseases or age.
How Minnesota’s system worked in practice
Minnesota’s weighted scoring system with race as a factor was in place from early December 2021 to early January 2022. It was used for less than a month of the 16 months the program operated.
We “did not use race/ethnicity during (the) lottery, when stuff was at its shortest,” Leider said. It “was used for a small time before that, based on clinical guidance, that showed being BIPOC was associated with worse outcomes even after controlling for comorbidities, age, what have you. But that went away before (the) lottery was needed.”
A case study Leider and other researchers published shows that 31,559 people received referrals through the program to get monoclonal antibody treatments to treat COVID-19 or for protection postexposure.
Of the 29,281 people who received it for treatment of the virus, at least 79% were white. About 11% declined to provide a race or ethnicity, and about 9% were people of color, including Black, Asian, American Indian, Native Hawaiian, Hispanic/Latino or other, the data shows.
Our ruling
Kirk claimed that in Minnesota, Walz rationed access to monoclonal antibody treatments for COVID-19 based on skin color, and that white people died because they were denied access.
For about a month during the pandemic, Minnesota did factor race into a scoring system to prioritize referrals for the treatments. A case study after the state’s program ended shows that at least 79% of patients who received referrals were white, in line with the racial composition of the state’s population.
People who were clinically eligible for the treatments weren’t denied access, but received referrals after higher-risk patients received theirs. By early 2022, when monoclonal antibody supplies were lowest and Minnesota used a weighted lottery system, race had been removed as a scoring factor.
We rate the claim Mostly False.
PolitiFact researcher Caryn Baird contributed to this fact check.
This fact check was originally published by PolitiFact, which is part of the Poynter Institute. See the sources for this fact check here.