 Covering COVID-19 is a daily Poynter briefing of story ideas about the coronavirus and other timely topics for journalists, written by senior faculty Al Tompkins. Sign up here to have it delivered to your inbox every weekday morning.
Covering COVID-19 is a daily Poynter briefing of story ideas about the coronavirus and other timely topics for journalists, written by senior faculty Al Tompkins. Sign up here to have it delivered to your inbox every weekday morning.
Readers, I am going to spend today’s entire newsletter deeply exploring two key issues. This post is a little longer than normal but I hope you will see it is meant to explain these fairly complex issues.
I am going to give you the resources you will need whenever the Supreme Court makes its important ruling on whether the Occupational Safety and Health Administration has the legal authority to mandate vaccines and testing in workplaces. And I am going to explore the question of exactly how many children are hospitalized with COVID-19, which is only debatable because the data is so unclear.
Decision day? Businesses and 80 million workers await a Supreme Court decision on the COVID-19 vaccination/testing mandate
Today was the day that OSHA was to have started requiring all employers with 100 or more workers to begin enforcing rules that would require employees to either be vaccinated against COVID-19 or undergo weekly testing.
OSHA indicated it would move slowly on enforcing the vaccine regulations while the U.S. Supreme Court considers whether OSHA has the legal authority to enforce the rule ordered by President Joe Biden. The ruling could come at any moment.
Companies that fail to comply with the order to have workers fully vaccinated by today could face fines in the range of $14,000. That figure could go higher for companies that willfully violate the order.
The new order says employers will have the burden of determining the vaccine status of all employees, meaning they will have to see proof of vaccination and maintain records. It says employers must, “Require employees to provide prompt notice when they test positive for COVID-19 or receive a COVID-19 diagnosis. Employers must then remove the employee from the workplace, regardless of vaccination status; employers must not allow them to return to work until they meet required criteria.”
The court also will decide whether the federal government has the authority to force health care workers to be vaccinated without an option to stay unvaccinated and routinely test for the virus.
Based on the tone and content of the justices’ questions during a Friday hearing, there seemed to be less concern about mandating vaccines for health care workers than for everyone else. But some justices hinted that it may be an overreach for OSHA to require vaccinations as a means of making workplaces safe.
Chief Justice John Roberts indicated that he believes that states and Congress should address the issue of workplace safety and that if Congress intends for OSHA to have this level of workplace oversight, it should say so.
“It’s not our role to decide public health questions,” Justice Neil Gorsuch said. “But it is our role to decide who should decide.”
Justices Elena Kagan, Stephen Breyer and Sonia Sotomayor all said that the pandemic is an extraordinary threat that requires the kind of enforcement that OSHA was to have started today.
The key to the case
Here, again, is a reference I provided when OSHA first issued its order to employees that spelled out what the Biden administration says gives it the authority to impose the mandate for vaccination or testing.
The OSHA order says, in effect, that where there is a potential “grave danger” to employees, the government has the obligation and authority to protect them, and that Congress has granted OSHA virtually unlimited discretion to keep workers safe. The below passage was part of OSHA’s order to employers and is the cornerstone of its defense before the Supreme Court. I include the citation here because it will, in all probability, be key to the court’s ruling. I bolded some key passages.
The purpose of the Occupational Safety and Health Act of 1970 (OSH Act), 29 U.S.C. 651 et seq., is “to assure so far as possible every working man and woman in the Nation safe and healthful working conditions and to preserve our human resources.” 29 U.S.C. 651(b). To this end, Congress authorized the Secretary of Labor (Secretary) to promulgate and enforce occupational safety and health standards under sections 6(b) and (c) of the OSH Act.1 29 U.S.C. 655(b). These provisions provide bases for issuing occupational safety and health standards under the Act. Once OSHA has established as a threshold matter that a health standard is necessary under section 6(b) or (c)—i.e., to reduce a significant risk of material health impairment, or a grave danger to employee health—the Act gives the Secretary “almost unlimited discretion to devise means to achieve the congressionally mandated goal” of protecting employee health, subject to the constraints of feasibility. See United Steelworkers of Am. v. Marshall, 647 F.2d 1189, 1230 (D.C. Cir. 1981)
A standard’s individual requirements need only be “reasonably related” to the purpose of ensuring a safe and healthful working environment. Id. at 1237, 1241; see also Forging Indus.
Ass’n v. Sec’y of Labor, 773 F.2d 1436, 1447 (4th Cir. 1985). OSHA’s authority to regulate employers is hedged by constitutional considerations and, pursuant to section 4(b)(1) of the OSH Act, the regulations and enforcement policies of other federal agencies. See, e.g., Chao v. Mallard Bay Drilling, Inc., 534 U.S. 235, 241 (2002).
The OSH Act in section 6(c)(1) states that the Secretary “shall” issue an emergency temporary standard (ETS) upon a finding that the ETS is necessary to address a grave danger to workers. See 29 U.S.C. 655(c). In particular, the Secretary shall provide, without regard to the requirements of chapter 5, title 5, United States Code, for an emergency temporary standard to take immediate effect upon publication in the Federal Register if the Secretary makes two determinations: That employees are exposed to grave danger from exposure to substances or agents determined to be toxic or physically harmful or from new hazards, and that such emergency standard is necessary to protect employees from such danger. 29 U.S.C. 655(c)(1).
The reality is that OSHA likely does not have enough inspectors to vigorously inspect and enforce this rule. NPR points out that OSHA will have to rely on worker complaints to find noncompliant companies. According to OSHA, there are about 1,850 federal and state inspectors covering some 8 million worksites nationwide.
How many children are hospitalized with or because of COVID-19?
During the Supreme Court hearing on vaccine/testing mandates, Justice Sotomayor stunned listeners when she said, “We have hospitals that are almost at full capacity with people severely ill on ventilators. We have over 100,000 children, which we’ve never had before, in serious condition, many on ventilators.”
Nobody seems to know where she came up with that number, but the truth is certainly nowhere close to that many children hospitalized or in serious condition from COVID-19. I will show you how difficult it is to know the true number, but know that it is likely closer to 3,700 children. That’s a lot, and it is also not 100,000.
I do not mean to hint that pediatric COVID-19 cases are not rising or are unconcerning; they are both concerning and rising. But the exact number is elusive because states do not uniformly report the figures in a timely way. We can discern, as I will show you, that cases are rising, but the numbers are so fluid that journalists default to reporting the increase in pediatric COVID-19 hospitalizations as a percentage rather than a raw number. Or in some cases, journalists just repeat the descriptions from health officials who say the pediatric infections are “skyrocketing, exploding, climbing and filling pediatric ICUs.”
To complicate matters, some states stopped reporting demographics, many states report age groups differently and data is woefully slow to arrive.
Percentages are not terribly useful when the baseline number is small and a small number is added to it. (If you start with one case and then another case comes in, you have a 100% increase, though you are not being overrun with new cases.)
We can get up-to-date data on how many COVID-19 cases are detected and, for certain, the number is rising. Right now, something close to one out of 10 children in the U.S. has tested positive for COVID-19 since the start of the pandemic, according to the American Academy of Pediatrics. But since children tend not to get severely ill from COVID-19, positive cases may not be the most important number, except that it might speak to the urgent need to safely vaccinate younger children.
The AAP says 0.1%-1.6% of children who test positive to COVID-19 require hospitalization. If that number holds through the omicron wave, then you could predict how many pediatric hospitalizations we might have from the number of positive cases, and the prediction is that it will rise.
The American Academy of Pediatrics says:
COVID-19 cases among US children have reached the highest case count ever reported since the start of the pandemic. For the week ending December 30th, over 325,000 child COVID-19 cases were reported. This number is a 64% increase over the 199,000 added cases reported the week ending December 23rd and an almost doubling of case counts from the two weeks prior.
The Associated Press expressed the rise in pediatric COVID-19 cases as a comparison of cases per population: “Since mid-December, with the highly contagious omicron variant spreading furiously around the country, the hospitalization rate in these youngest kids has surged to more than 4 in 100,000 children, up from 2.5 per 100,000.”
One problem is that states seem to report cases by different age groups. One state reports it as 0-4 years old, another 0-11. The Centers for Disease Control and Prevention’s figures are based on data from drawn from over 250 hospitals in 14 states. So, again, there is no solid national figure. Why?
On Jan. 3, admissions were running at around 1,354 per day, NBC News said. NBC News did its own analysis of the state-supplied data it could find and says nine states have reported record numbers of COVID-related pediatric hospitalizations: Connecticut, Georgia, Illinois, Kentucky, Massachusetts, Maine, Missouri, Ohio and Pennsylvania, as well as Washington, D.C.
To give you a sense of scale, Children’s Hospital New Orleans said it had seen a spike in children who have COVID-19 and it is currently treating 14 children, three of them in intensive care. In the first week of January, Texas Children’s Hospital in Houston counted close to 70 pediatric COVID-19 patients.
Here is an update from South Carolina’s children’s hospitals:
ALL 35 CHILDREN admitted to South Carolina Children’s Hospitals with COVID are UNVACCINATED. Every one. Of those, 14 are not eligible because they are too young. 10 children are critically ill from the virus in ICU. One is on life support. #GetVaccinatedNow pic.twitter.com/lld839Inyz
— Cleavon MD
(@Cleavon_MD) January 8, 2022
The American Academy of Pediatrics says:
A smaller subset of states reported on hospitalizations and mortality by age; the available data indicate that COVID-19-associated hospitalization and death is uncommon in children.
At this time, it appears that severe illness due to COVID-19 is uncommon among children.
The AP said during the last week of December, “The average number of under-18 patients admitted to the hospital per day with COVID-19 was 766, double the figure reported just two weeks ago.” And, the AP added this important passage:
The CDC also said the surge could be partially attributable to how COVID-19 hospitalizations in this age group are defined: a positive virus test within 14 days of hospitalization for any reason.
The severity of illness among children during the omicron wave seems lower than it was with the delta variant, said Seattle Children’s Hospital critical care chief Dr. John McGuire.
“Most of the COVID+ kids in the hospital are actually not here for COVID-19 disease,” McGuire said in an email. “They are here for other issues but happen to have tested positive.”
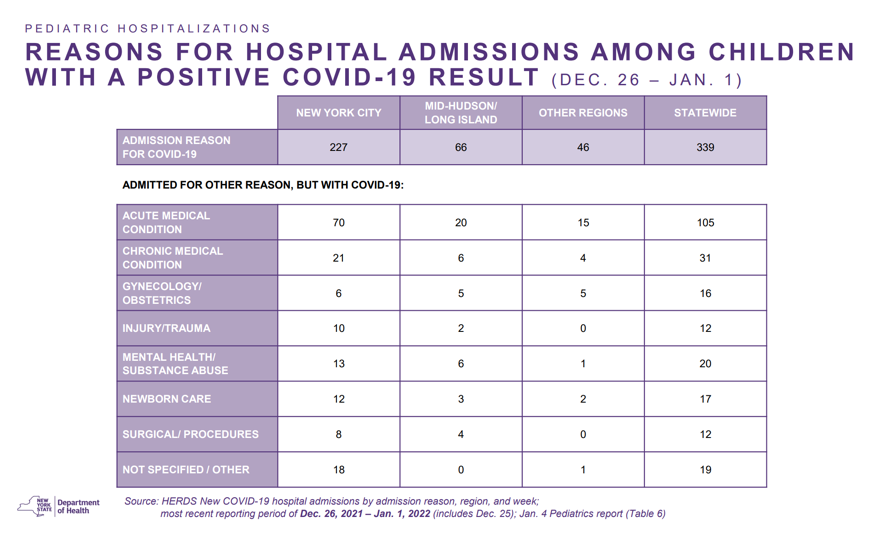
But that is not what is happening in New York. The New York Department of Health provides a comprehensive report of pediatric infections and hospitalizations, even though the latest data is still more than a week old. But the data is interesting because it shows the number of children who were hospitalized with COVID-19 rather than being hospitalized for something else and then testing positive for COVID-19. As you can see, both in New York City and statewide in New York, most of the COVID-19 cases were children who came in sick with COVID-19, not with other medical issues as the primary reason for hospitalization.
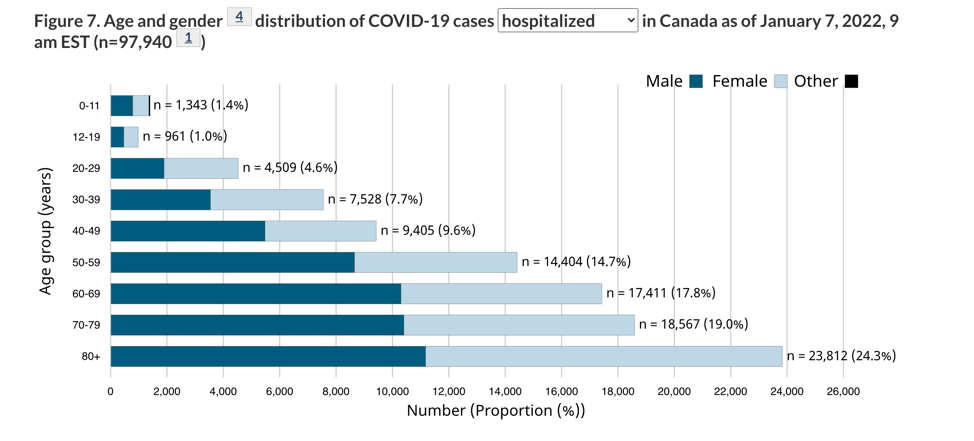
Canada makes the data much clearer than the U.S. The Canadian government posts daily updates like this showing nationwide, last week, 1,343 0-11 year-olds were hospitalized with COVID-19 in Canada. That is about 1.4% of all cases there.
The CDC does provide a sort of snapshot of data from 14 states representing about 10% of the U.S. population. While this is not as solid as Canada’s hard data, it is reflective of what we would find if we did have hard data from the rest of the country. At least it could be useful in spotting trends. And this is what that chart shows — notice the tiny yellow tip of each column, which is the pediatric cases.
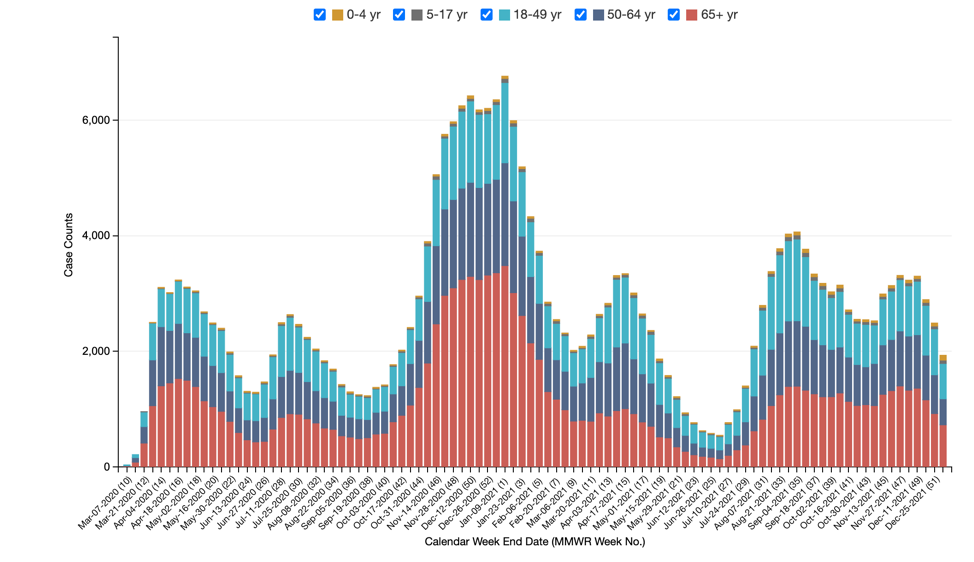
(CDC)
That chart shows the raw number of cases. But now let’s look at the same data expressed as a percentage of cases. You will see the yellow tip of the column grew in the last weeks of the year. It means that pediatric patients make up a greater percentage of people in the hospital.
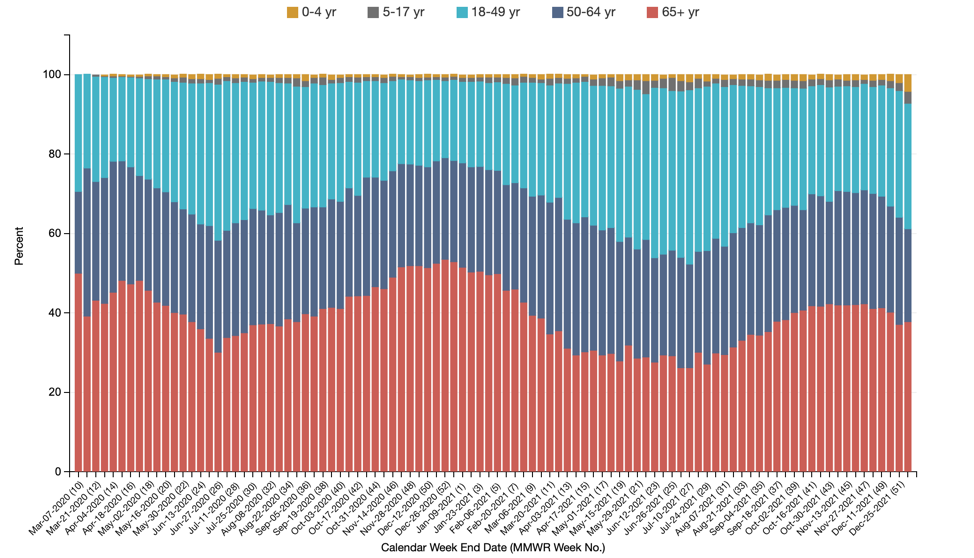
(CDC)
Let’s zoom in on two columns that tell a key story. The last column shows that the week of Dec. 25, about 4% of COVID-19 hospitalizations were children under the age of 5. Just the week before, it was half that many.
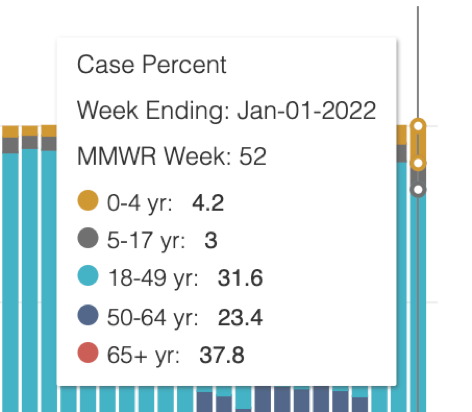
(CDC)
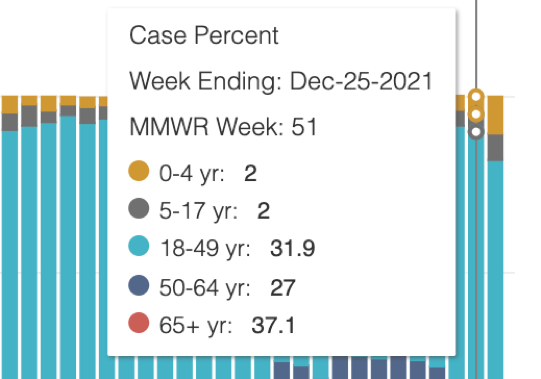
(CDC)
Make no mistake, pediatric COVID-19 cases can be severe. A study from this summer of pediatric patients in six hospitals found hospitalization rates rose during the delta variant spike. A third of the children admitted were under age 5, which is the group that still has no approved vaccine to protect against severe COVID-19. The report said more than three-quarters — 78% — were hospitalized because of complications of COVID-19. About half needed help breathing, and nearly a third were placed in intensive care. It appears that the omicron variant is sending even more children to the hospital, although with less severe complications, but sick enough to be hospitalized all the same.
I should add that pediatric hospitalizations, like adult hospitalizations, are largely among the unvaccinated.
While it does not tell us how many children are in ICUs, the Department of Health and Human Services does provide a daily dashboard of hospital capacity. This data from the weekend shows 18% of hospital beds (138,073) are being used by COVID-19 patients. Overall, hospitals are running about 79% capacity. You can zoom into your state going here. Look for the state/territory search box in the upper right corner of the graphic.
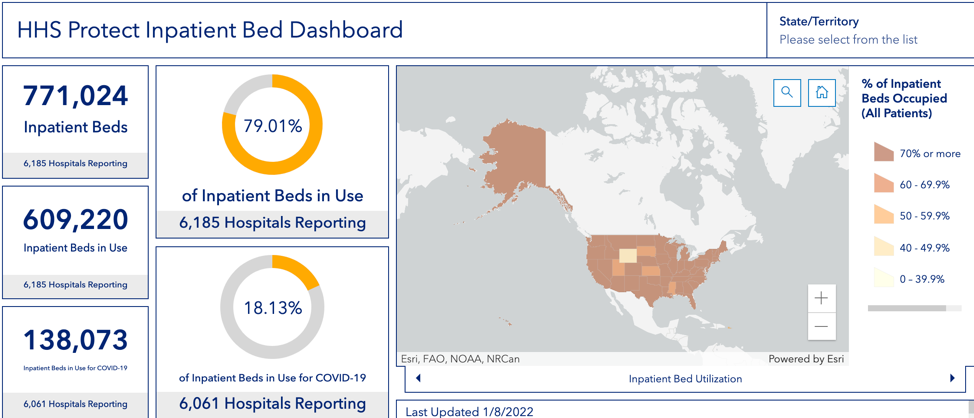
(HHS)
You could use the projected percentages that the CDC gives us of pediatric cases and estimate how many are in hospital beds and ICUs, but that is more guesswork than reporting.
The HHS data shows that ICU wards nationwide are running at about 80% capacity, with 22,394 ICU beds being used by COVID-19 patients.
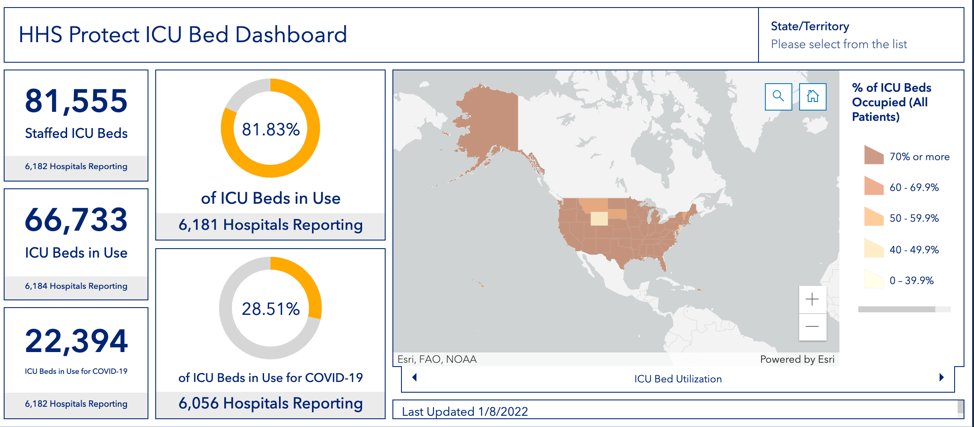
(HHS)
As I look through the data from states this weekend:
- Arkansas’s ICUs were at 87% capacity and 29% were COVID-19 cases.
- Alabama is at 89% ICU capacity with 21% of them COVID-19 cases.
- Delaware is at 87% ICU capacity with a third of the patients being treated for COVID-19.
- Georgia’s ICUs are 86% full with 31% of them COVID-19 patients
- Indiana’s ICUs are at 87% capacity with 49% of the patients being treated for COVID-19.
- Iowa’s ICUs are 85% full with 32% of the ICU patients infected with COVID-19.
- Kansas is at 84% ICU capacity with 32% of the ICU patients infected with COVID-19.
- Kentucky’s ICUs are 91% full and 29% of the beds have COVID-19 patients.
- Massachusetts’ ICUs are 86% in use with 31% of them being used for COVID-19 cases.
- Michigan’s ICU’s are 85% full and 34% of those cases are COVID-19.
- Minnesota’s ICUs are 87% full with 29% of the ICU beds being COVID-19 cases.
- Mississippi’s ICU’s are 86% in use with 26% of the cases being COVID-19 cases. Note this is a smaller percentage than most of the other highly infected states.
- Missouri’s ICUs are 91% full with 38% of the cases, 692 beds, being used for COVID-19.
- Nebraska’s ICU beds are 86% full with 29% of the cases related to COVID-19.
- Nevada’s ICU beds are 86% full with 26% of the cases related to COVID-19.
- New Hampshire’s ICU beds are 90% full with 32% of the beds devoted to COVID-19 cases.
- New Mexico’s ICU beds are 90% of capacity with 35% of the ICU beds being used by COVID-19 patients.
- Ohio’s ICU beds are 85% filled with 36% of them used for COVID-19 cases.
- Oklahoma’s ICU beds are 86% full with 31% of them being used for COVID-19 cases.
- Rhode Island reports 86% of ICUs in use with 38% of beds being used for COVID-19.
- Texas’ ICUs are 90% full with 28% of the ICU beds (1,821) being used for COVID-19 cases.
- A number of other states had ICU use in the low to mid 80%. One state, Wyoming, reports 47% of ICU beds in use with 16% of those beds (18 beds) being used to treat COVID-19 patients.
There are so many reasons that states should be routinely reporting this data (as Canada does) and so many politically motivated reasons why they do not. Journalists should be pounding away with questions every day demanding this data. Without it, we could be missing important trends, and deniers use the lack of specific data to claim the pandemic is overblown.
Children who get COVID risk developing diabetes
A new CDC report says children who recovered from COVID-19 have an increased risk of Type 1 or Type 2 diabetes. Previous studies showed adults who had COVID-19 also have a higher diabetes risk.
This new research is based on insurance claims that showed an increasing number of claims for children with diabetes after they were treated for COVID-19. The study included two dozen hospitals in 20 states.
But two different insurance claim databases showed wildly different results. One database showed that pediatric COVID-19 patients were more than 30% more likely to develop diabetes than non-COVID infected kids. Another database said the increased likelihood of developing diabetes could be as high as 166% in children who get sick with COVID-19.
Typically, the diabetes diagnosis came about a month after the patient recovered from COVID-19. Doctors say they are not sure if these diabetes cases will be lifelong conditions or whether the child will outgrow them.
Finally, this data from the weekend
Amarillo, Texas. All 39 people on LIFE SUPPORT due to COVID are UNVACCINATED. Every one. #GetVaccinatedNow pic.twitter.com/adrra3buan
— Cleavon MD
(@Cleavon_MD) January 8, 2022
We’ll be back tomorrow with a new edition of Covering COVID-19. Are you subscribed? Sign up here to get it delivered right to your inbox.